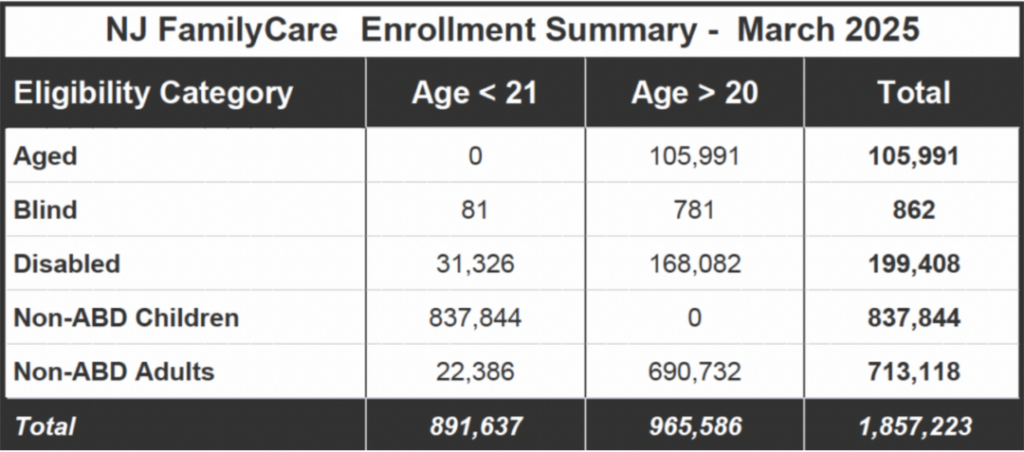
As New Jersey lawmakers work on the next budget, Congress is considering deep cuts to federal programs, including Medicaid. Strengthening New Jersey’s Medicaid program is a central focus of the Quality Institute and critical to our members. Medicaid is the largest overall funder of health care services in New Jersey. The program’s mission is to ensure that children, people with disabilities, those who are pregnant, the elderly, and people with no-to-low-income have access to essential health care. Today, New Jersey Medicaid covers about 1.8 million people, including one in three children. The program is jointly funded, with a current annual overall cost of $24 billion, comprised of $14 billion from federal funds and $10 billion in state funds (Details on who is covered and a breakdown of expenditures can be found in Charts no.1 and 2).
Chart 1
Chart 2
If the proposed cuts are enacted, the impact will be painful and unprecedented. The New Jersey Department of Human Services created a comprehensive review of each of the proposed cuts being considered by Congress and outlined how each would directly reduce the $14 billion in federal funds New Jersey currently receives. These cuts are so large that the state will not be able to replace the lost funds – meaning people would lose Medicaid coverage or benefits would be drastically reduced.
The claims from Congressional lawmakers and federal officials that the cuts could come from fraud, waste, and abuse (FWA) are purposefully disingenuous. Directly cutting a program — and then saying the cuts can come from fraud, waste, and abuse savings — is a flimsy cover when done without showing how any of the cuts address fraud, waste and abuse in the program. If the federal government is sincere about cutting FWA, it would not have fired the HHS Inspector General. Instead, it would review the many audit reports issued by state and federal inspector generals and oversight agencies and pursue strategies to fight fraud, waste and abuse by providing staffing, data, and other targeted supports. The irony is deep cuts to Medicaid would likely result in cuts to fraud-fighting initiatives.
While we hope that well-informed minds and consciences prevail and the proposed cuts will not come about, that doesn’t mean that state policy makers should accept the Medicaid program’s status quo. With its current fiscal challenges and needs, now is the time to strengthen the current Medicaid system to be more efficient, transparent, and focused on fundamental care. This means a rightsizing of spending on care with the greatest value, such as comprehensive primary and preventive care, including maternal and reproductive health, integrated mental health, and preventive oral health. We must invest more, not less, on the care that keeps people healthier, identifies issues earlier, and is delivered in the community.
For too long, the reimbursement rates in NJ FamilyCare for these fundamental services have been too low, resulting in low access, delays in care, and overuse of emergency departments and other higher cost settings to manage avoidable acute, chronic, and complex health care issues.
As the budget processes at the state and federal levels continue, we look forward to sharing our vision for a stronger Medicaid system and a healthier state. We want to hear your ideas as well. There is work we can do together to improve access and quality. Honesty and realism are needed at the table. We look forward to having those productive discussions together.